We know that when an older adult falls, there is a high likelihood of injury. Could we address reducing the rate of falls a bit differently in the clinic?
 If you sit back and think of what you would typically observe in a treatment session focused on improving balance, you would typically see activities that seem more anticipatory in nature. For lack of a better description, you’d notice postural sway with the movement revolving around the ankle joint. Usually the person is in a static position.
If you sit back and think of what you would typically observe in a treatment session focused on improving balance, you would typically see activities that seem more anticipatory in nature. For lack of a better description, you’d notice postural sway with the movement revolving around the ankle joint. Usually the person is in a static position.
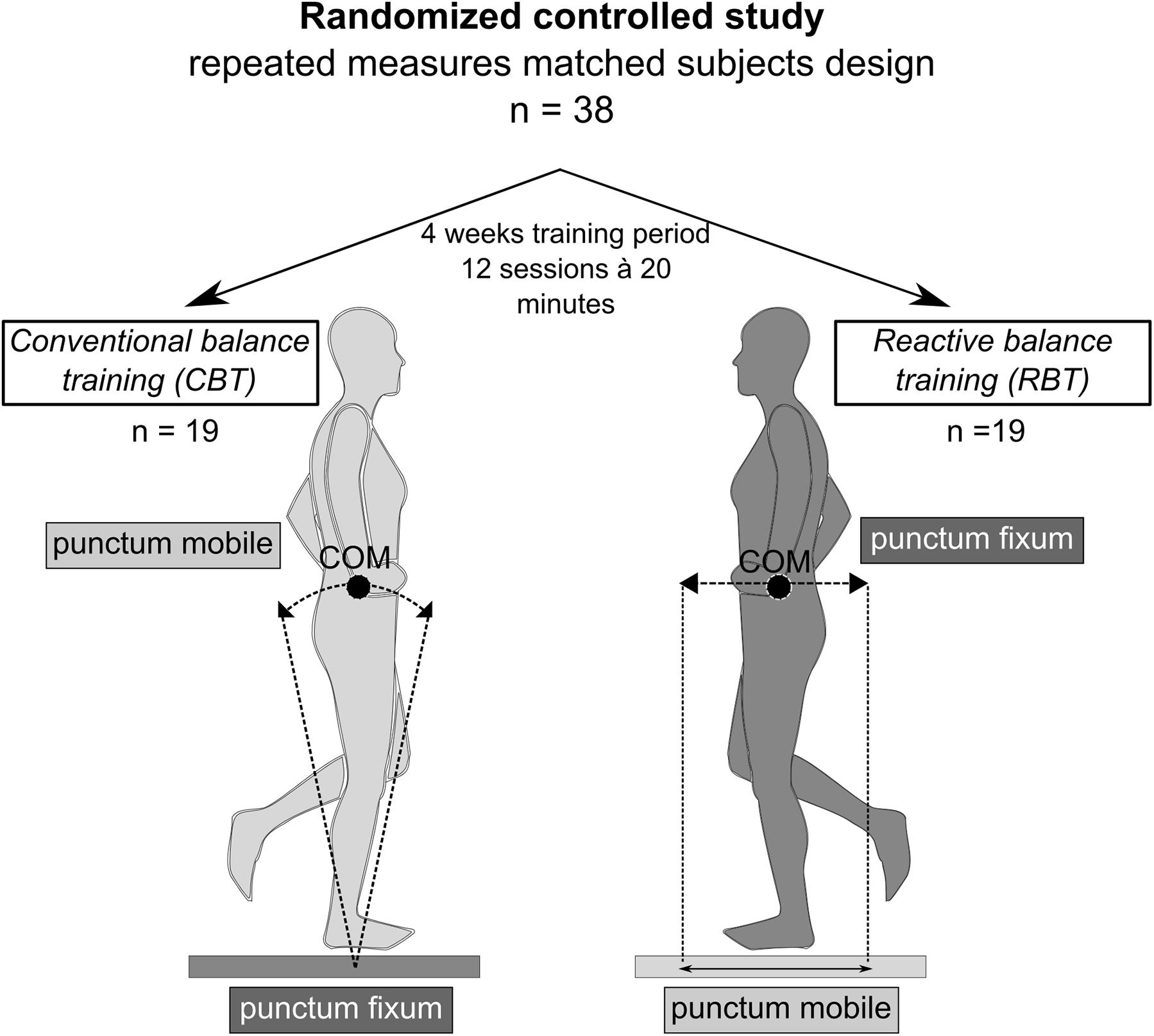
I took liberty to snag the image from the research study. I had to do this because this image is far better than any words I could use to describe reactive balance training. Conventional balance training, in my opinion, typically heavily relies on anticipatory activities. This study begins to look at reactive balance training. Reactive balance training is different because something is done to the patient and the patient has to provide a reflexive response to eliminate experiencing a fall.
In this particular study, the reactive balance training would be considered dynamic. The subjects were exposed to a “slip” situation. The platform below the foot was moved forward or backward or in various directions to capture the response. In other words, these subjects were able to experience a fall situation and respond.
You’ll find the abstract to the recent study below.
Neuromuscular and Kinematic Adaptation in Response to Reactive Balance Training – a Randomized Controlled Study Regarding Fall Prevention.
Abstract
Slips and stumbles are main causes of falls and result in serious injuries. Balance training is widely applied for preventing falls across the lifespan. Subdivided into two main intervention types, biomechanical characteristics differ amongst balance interventions tailored to counteract falls: conventional balance training (CBT) referring to a balance task with a static ledger pivoting around the ankle joint versus reactive balance training (RBT) using externally applied perturbations to deteriorate body equilibrium. This study aimed to evaluate the efficacy of reactive, slip-simulating RBT compared to CBT in regard to fall prevention and to detect neuromuscular and kinematic dependencies.
In a randomized controlled trial, 38 participants were randomly allocated either to CBT or RBT. To simulate stumbling scenarios, postural responses were assessed to posterior translations in gait and stance perturbation before and after 4 weeks of training. Surface electromyography during short- (SLR), medium- (MLR), and long-latency response of shank and thigh muscles as well as ankle, knee, and hip joint kinematics (amplitudes and velocities) were recorded.
Both training modalities revealed reduced angular velocity in the ankle joint (P < 0.05) accompanied by increased shank muscle activity in SLR (P < 0.05) during marching in place perturbation. During stance perturbation and marching in place perturbation, hip angular velocity was decreased after RBT (P from TTEST, Pt < 0.05) accompanied by enhanced thigh muscle activity (SLR, MLR) after both trainings (P < 0.05). Effect sizes were larger for the RBT-group during stance perturbation. Thus, both interventions revealed modified stabilization strategies for reactive balance recovery after surface translations.
Characterized by enhanced reflex activity in the leg muscles antagonizing the surface translations, balance training is associated with improved neuromuscular timing and accuracy being relevant for postural control. This may result in more efficient segmental stabilization during fall risk situations, independent of the intervention modality. More pronounced modulations and higher effect sizes after RBT in stance perturbation point toward specificity of training adaptations, with an emphasis on the proximal body segment for RBT. Outcomes underline the benefits of balance training with a clear distinction between RBT and CBT being relevant for training application over the lifespan.
{{cta(‘c6ecd159-44e1-4eb3-9940-fbb5cb2761d5’)}}

Leave a Reply